Last updated: June 04, 2012
International Effort Finds New Genetic Variants Associated with Lipid Levels, Risk for Coronary Artery Disease

International Effort Finds New Genetic Variants Associated with Lipid Levels, Risk for Coronary Artery Disease
 Bethesda, Md., Sun., Jan. 13, 2008 — Environmental and genetic factors influence a person's blood fat, or lipid levels, important risk factors for coronary artery disease (CAD). While there is some understanding of the environmental contribution, the role of genetics has been less defined. Now, in an international collaboration supported primarily by the National Institutes of Health (NIH), scientists have discovered more than 25 genetic variants in 18 genes connected to cholesterol and lipid levels. Seven of the 18 genes previously had not been connected to these levels, while the 11 others confirm previous discoveries. In the investigation, published online January 13 and in the February print issue of Nature Genetics, the associated genes were found through studies of more than 20,000 individuals and more than 2 million genetic variants, spanning the entire genome. These variants potentially open the door to strategies for the treatment and prevention of CAD.
Bethesda, Md., Sun., Jan. 13, 2008 — Environmental and genetic factors influence a person's blood fat, or lipid levels, important risk factors for coronary artery disease (CAD). While there is some understanding of the environmental contribution, the role of genetics has been less defined. Now, in an international collaboration supported primarily by the National Institutes of Health (NIH), scientists have discovered more than 25 genetic variants in 18 genes connected to cholesterol and lipid levels. Seven of the 18 genes previously had not been connected to these levels, while the 11 others confirm previous discoveries. In the investigation, published online January 13 and in the February print issue of Nature Genetics, the associated genes were found through studies of more than 20,000 individuals and more than 2 million genetic variants, spanning the entire genome. These variants potentially open the door to strategies for the treatment and prevention of CAD.
"Heart disease is a leading cause of illness, disability and death in industrialized countries, particularly for older people," says National Institute on Aging (NIA) Director Richard J. Hodes, M.D. "We know that certain lifestyle factors like smoking, diet and physical activity greatly affect a person's lipid profiles. This study is an important, basic step in finding the genes that influence lipid levels and heart disease so that we can better understand the genetic contribution to cardiovascular risk."
Cristen Willer, Ph.D., at the University of Michigan's School of Public Health, Ann Arbor, and Serena Sanna, Ph.D., at the C.N.R. Institute of Neurogenetics and Neuropharmacology, Monserrato, Italy, and other members of the SardiNIA Study of Aging, including investigators at NIA, conducted the study, along with members of the Finland-United States Investigation of Non-Insulin-Dependent Diabetes Mellitus Genetics (FUSION) study, which included investigators in North Carolina, Michigan, Finland, Los Angeles and from the National Human Genome Research Institute (NHGRI). SardiNIA and FUSION investigators also coordinated the efforts of other groups in France, the United Kingdom and across the United States.
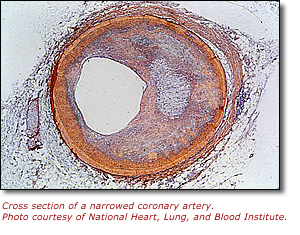
The purpose of the study was to identify comprehensively genetic variants that influence lipid levels and to examine the relationships between these genetic variants and risk of CAD. High levels of low-density lipoprotein (LDL) ("bad" cholesterol) appear to increase the risk of CAD by narrowing or blocking arteries that carry blood to the heart. High levels of high-density lipoprotein (HDL) ("good" cholesterol) appear to lower the risk. High levels of triglycerides, which make up a large part of the body's fat and are also found in the bloodstream, are also associated with increased risk of CAD.
To identify genetic variants that play a role in lipid levels, researchers turned to a relatively new approach, known as a genome-wide association study (GWAS). The GWAS strategy enables researchers to survey the entire human genetic blueprint, or genome, not just the genetic variants in a few genes. The human genome contains approximately 3 billion base pairs, or letters, of DNA. Small, single-letter variations naturally occur about once in every 1,000 letters of the DNA code. Most of these genetic variants have not yet been associated with particular traits or disease risks. However, in some instances, people with a certain trait, such as higher levels of LDL cholesterol, tend to have one version of the variant, while those with lower levels are more likely to have the other version. In such instances, researchers may infer that there is an association between the values of the trait and the variants in the gene.
Typically, GWAS studies have been carried out in samples where all individuals are examined with the same gene chip, an experimental device that allows investigators to measure more than 100,000 genetic variants in a single experiment. But in this study, investigators developed and employed new statistical methods that allowed them to combine data across different gene chips and thus examine much larger numbers of participants.
With the statistical power gained by new programs that facilitated pooling of the large SardiNIA, FUSION and Diabetes Genetic Initiative (DGI) datasets, researchers were able to identify variations in 18 genes that influence HDL, LDL and/or triglyceride levels. This list of lipid-associated genes is substantially longer than what was generated by analyses of individual datasets, which had only pointed to one to three genes each. Of the seven newly implicated genes, two were associated with HDL levels, one with LDL levels, three with triglyceride levels and one with both triglycerides and LDL levels. A summary of the data is available online at www.sph.umich.edu/csg/abecasis/public/lipids.
"These results are yet another example of how genome-wide association studies are opening exciting new avenues for biomedical research," says NHGRI Director Francis S. Collins, M.D., Ph.D., who is a coauthor of the study and an investigator in NHGRI's Genome Technology Branch. "While some of the genetic variants we identified are known to play a well-established role in lipid metabolism, others have no obvious connection. Further studies to identify the precise genes and biological pathways involved could shed new light on lipid metabolism."
Scientists estimate that the genetic contribution to lipid levels is about 30 to 40 percent; the genetic variants uncovered in the new study are responsible for about 5 to 8 percent of that contribution, the scientists note, which means there is more work to be done. "In this study we carried out a comprehensive search for common variants of large effect. The genetic factors still to be discovered might turn out to be common variants with smaller effects or rare variants with a large effect," says Karen L. Mohlke, Ph.D., of the University of North Carolina, Chapel Hill, who co-directed the study with Gonçalo R. Abecasis, Ph.D., of the University of Michigan's School of Public Health.
To determine if the genetic variants associated with lipid levels also influence risk of heart disease, the researchers compared their results with results from the Wellcome Trust Case Control Consortium's recent genome-wide association study of CAD involving 15,000 British individuals. They found that all gene variants associated with increased LDL levels also were more prevalent among people with CAD. People with the gene variant for high triglyceride levels also had an increased risk for CAD, although the relationship was not as strong. No relationship was found between HDL and CAD.
"It was surprising that while it was clear that genetic variants that increase your 'bad' cholesterol are also associated with increased risk of heart disease, we did not find that variants influencing your 'good' cholesterol were associated with decreased risk of coronary artery disease. Perhaps that result will lead us to re-examine the roles of good and bad cholesterol in susceptibility to heart disease," remarks Abecasis.
Identifying a correlation among genes influencing lipid levels and risk for coronary heart disease is a first step in a long path to potentially important clinical implications. "What we're looking for, ultimately, are novel therapeutics and/or life-style modifications that can be recommended to individuals to help manage blood lipid levels and reduce risk of heart disease," says David Schlessinger, Ph.D., chief of the NIA's Laboratory of Genetics and NIA Project Officer for SardiNIA.
This study also demonstrates the power of international collaboration in genetic analyses. None of the studies that cooperated to make this work possible were large enough to find all of these important associations alone. By working together, previously unsuspected genetic influences on lipid levels and heart disease were revealed.
SardiNIA is funded by NIA and FUSION receives support from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and NHGRI. Additional genetic data were provided by DGI, which involves Finnish and Swedish individuals and is a collaboration of the Broad Institute of Harvard and MIT, Cambridge, Mass.; Lund University, Malmo, Sweden; and Novartis, Basel, Switzerland.
In addition to the NIA; NHGRI; University of Michigan, Ann Arbor; University of North Carolina, Chapel Hill; Department of Health and Functional Capacity, National Public Health Institute, Helsinki, Finland; Keck School of Medicine, University of Southern California, Los Angeles; and the C.N.R Institute of Neurogenetics and Neuropharmacology, other institutions with researchers taking part in the study were: Geriatrics Operating Unit, Institute for the Endocrine and Metabolic Pathology, Rome; Clinical Trials Services Unit, University of Oxford, England; National Center of Genotypage, Genomic Institute, Commissionership of Atomic Energy, Evry, France; Department of Social Medicine, University of Bristol, England; University of Maryland School of Medicine, Baltimore; Departments of Public Health and of Medical Data Processing, School of Medicine, Paris; Research Unit of Nutritional Epidemiology, Bobigny, France; London School of Hygiene and Tropical Medicine, University of London; and Department of Public Health, University of Helsinki, Finland.
Data used in this analysis were generated by studies supported by NIA, NHGRI, NIDDK and the National Heart, Lung and Blood Institute (NHLBI), all part of NIH; the Wellcome Trust; the American Diabetes Association; the Department of Veteran Affairs; the British Heart Foundation; the United Kingdom's Medical Research Council; and the French Ministry of Higher Education and Research. The genome-wide scans of the FUSION participants' DNA were performed at the Center for Inherited Disease, using funding from NIH and Johns Hopkins University, Baltimore.
Also today, another NIH-supported genome-wide association study involving the SardiNIA, FUSION and DGI groups was released in the advance online publication of Nature Genetics. In this study, an international team, including many researchers from the lipid investigation, found evidence that common genetic variants recently linked to osteoarthritis may also play a minor role in human height.
For consumer information on heart disease, visit the NHLBI Web site at www.nhlbi.nih.gov/health/public/heart/index.htm.
The NIA leads the federal government effort conducting and supporting research on the biomedical and social and behavioral aspects of aging and the problems of older people. For more information on aging-related research and the NIA, please visit the NIA Web site at www.nia.nih.gov.
The National Institute of Diabetes and Digestive and Kidney Diseases, a component of the NIH, conducts and supports research in diabetes and other endocrine and metabolic diseases; digestive diseases, nutrition, and obesity; and kidney, urologic, and hematologic diseases. Spanning the full spectrum of medicine and afflicting people of all ages and ethnic groups, these diseases encompass some of the most common, severe, and disabling conditions affecting Americans. For more information about NIDDK and its programs, see www.niddk.nih.gov.
NHGRI's Division of Intramural Research develops and implements technology to understand, diagnose and treat genomic and genetic diseases. Additional information about NHGRI can be found at www.genome.gov. For more information about genome-wide association studies, go to www.genome.gov/20019523/genomewide-association-studies-fact-sheet/.
NIH — the nation's medical research agency — includes 27 institutes and centers and is a component of the U.S. Department of Health and Human Services. It is the primary federal agency for conducting and supporting basic, clinical and translational medical research, and it investigates the causes, treatments and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
To view the PDF on this page you will need Adobe Acrobat Reader. ![]()
Contacts
Megan Homer, NIA
301-496-1752
nianews3@mail.nih.gov
Geoff Spencer, NHGRI
301-402-0911
spencerg@mail.nih.gov
