Last updated: July 19, 2013
Genetic mystery of Behcet's disease unfolds along the ancient Silk Road

Genetic mystery of Behcet's disease unfolds along the ancient Silk Road
NIH researchers identify new gene variants associated with risk for complex inflammatory syndrome
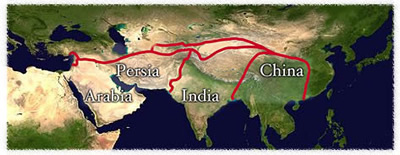 |
Named for the Turkish physician who described it in 1937, Behcet's (pronounced BET'-chets) disease is triggered by complex genetic and environmental factors, and causes inflammation of blood vessels in various parts of the body. Common symptoms include painful mouth and genital sores, and eye inflammation that can lead to blindness. In some cases, it can be life-threatening, affecting blood vessels in the brain, lungs, and other vital organs. About 1 in 250 people in Turkey have Behcet's disease; others with the disease are found largely in regions along the Silk Road.
Genetic factors are thought to play a role in susceptibility to Behcet's disease, with the human leukocyte antigen (HLA) B-51 gene region of the genome, accounting for about 20 percent of genetic risk for the disease. Researchers have been aware of the HLA B-51 association for about 40 years. Two years ago, the research team identified gene associations at two other specific chromosome locations, or loci.
"The current study represents an important advance because it dramatically broadens the spectrum of genetic loci associated with Behcet's disease," said Dan Kastner, M.D., Ph.D., scientific director of the Intramural Research Program at the National Human Genome Research Institute and senior author of the study. "These newly discovered genetic associations provide a link between Behcet's disease and other more common illnesses, and thereby suggest new therapies for Behcet's disease. In addition, two of the newly discovered genes provide an intriguing link between genes and the microbes in our environment."
Researchers conducted a genome-wide association study (GWAS) that enrolled 1,209 Turkish people affected by Behcet's disease and 1,278 unaffected Turkish people - all residents of the country. They looked at many points on the human genome called single-nucleotide polymorphisms (SNPs), with each SNP representing a difference in a single DNA building block, called a nucleotide. Researchers then compared SNP differences between people with and without disease.
From nearly 800,000 SNPs, researchers detected and mapped a small number that are found in those who have Behcet's disease at a significantly higher rate than in those without the disease, suggesting that the variant or another one nearby contributes to the disease.
"Each of the genetic factors may contribute a little to the overall risk of disease," said Elaine F. Remmers, Ph.D., staff scientist in NHGRI's Inflammatory Disease Section and study co-author. "We are also identifying them in pathways that are important in inflammatory disease development."
She noted that not all of the 800,000 gene variants analyzed were directly genotyped. Genotyping involves examining a person's DNA at a site where a variation is commonly known to occur. Instead, the team used the strategy of imputing, or surmising, that there were genotypes worth investigating near known variants.
"That worked very well for us," Dr. Remmers said. "We found that our predicted genotypes were pretty good and that the associations we found were quite similar in both the predicted and the experimentally confirmed genotypes."
Each of the four newly identified gene regions is already known to play a role in immune regulation. The genetic associations have helped classify Behcet's disease with more common inflammatory conditions such as psoriasis, inflammatory bowel disease and a form of spinal arthritis called ankylosing spondylitis.
Among the newly identified regions, researchers found:
- An important association between Behcet's disease and a gene called ERAP1. ERAP1 codes for a molecule that processes microbial proteins in white blood cells. Variants of this protein can lead to more or less efficient processing of microbial proteins before they are loaded onto HLA molecules for presentation to the immune system. The variants of ERAP1 identified in this study increase the risk of Behcet's disease, but only in those individuals with one specific HLA type, HLA-B51, which has previously been associated with Behcet's disease. Dr. Kastner speculates that the ERAP1 variant associated with Behcet's disease processes microbial proteins in such a way that they can be loaded onto the HLA-B51 molecule to trigger an abnormal immune response. The very same variant of ERAP1 that is associated with Behcet's disease is protective for ankylosing spondylitis and psoriasis, but only in people with the HLA types associated with those diseases.
- A significant association of Behcet's disease with variants near the CCR1 gene. Proteins coded by this gene help infection-fighting blood cells migrate to sites of invading microorganisms. When this function is defective, the microorganisms can trigger a persistent inflammatory response.
- An association of the disease with variants in the KLRC4 gene. The function of the receptor protein coded by this gene is not well understood, but the researchers suggest that it may be important to investigate further because it is located within the genomic region with the strongest evidence for linkage to a disease gene in a study of Turkish family health histories in which members sometimes have a rare familial form of Behcet's disease.
- An association with the STAT4 gene, in which different variants in the same vicinity of the genome increase risk for autoimmune diseases, including rheumatoid arthritis and lupus.
"We are incredibly excited about these latest findings," Dr. Kastner said. "Combined with our studies two years ago, the current genetic data make a strong case for a causal connection between Behcet's disease and disorders such as ankylosing spondylitis, psoriasis, and inflammatory bowel disease. This raises real hope that some of the treatments that have been found effective in these other illnesses will have some utility in Behcet's disease, thereby helping to alleviate suffering and prevent mortality.
For more about Behcet's disease, go to: www.niams.nih.gov/health_info/behcets_disease/
This research was supported by the intramural research programs of NHGRI; the National Institute of Arthritis and Musculoskeletal and Skin Diseases; the Center for Human Immunology, Autoimmunity and Inflammation at NIH; the Istanbul University Research Fund; the Japanese Ministry of Health, Labor, and Welfare; and the Japan Rheumatism Foundation.
NHGRI is one of the 27 institutes and centers at the NIH, an agency of the Department of Health and Human Services. The NHGRI Division of Intramural Research develops and implements technology to understand, diagnose and treat genomic and genetic diseases. Additional information about NHGRI can be found at its website, www.genome.gov.
The mission of the NIAMS, a part of the U.S. Department of Health and Human Services' National Institutes of Health (NIH), is to support research into the causes, treatment, and prevention of arthritis and musculoskeletal and skin diseases; the training of basic and clinical scientists to carry out this research; and the dissemination of information on research progress in these diseases. For more information about the NIAMS, call the information clearinghouse at (301) 495-4484 or (877) 22-NIAMS (free call) or visit the NIAMS website at www.niams.nih.gov
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 institutes and centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov
Contact
Raymond MacDougall
National Human Genome Research Institute
301-402-0911
macdougallr@mail.nih.gov
