"Until now, drugs used to treat Gaucher disease have not been able to enter the brain and reach those neurons that are affected in the most severe forms of Gaucher disease or in Parkinson's disease," said Dr. Sidransky. "It's really exciting to have found a molecule that theoretically could be widely available to treat people with these diseases. However, there's a long distance between identifying this molecule and having an approved drug." Dr. Sidransky has conducted research on Gaucher disease for the last 28 years and made the connection between Gaucher disease and Parkinson's disease in 2001.
Gaucher disease occurs when GBA1, the gene that codes for the protein glucocerebrosidase, is mutated. This protein normally helps cells dispose of certain fats (lipids), a type of waste produced by all cells. When a person inherits two mutated copies of GBA1, lipids accumulate and can cause symptoms such as enlargement of the spleen, frequent bleeding and bruising, weakened bones and, in the most severe cases, neurological disease. People with even one mutated copy of GBA1 are at higher risk of developing Parkinson's disease, a common disorder characterized by tremors, muscular rigidity and slowed movements.
 ]
]
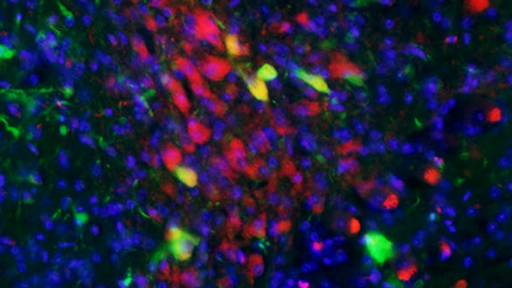
To better understand the connection between Gaucher and Parkinson's diseases, NHGRI researchers used a labor-intensive technology to develop pluripotent stem cells (unspecialized cells that can develop into various specialized body cells). Elma Aflaki, Ph.D., a research fellow in Sidransky's lab, created stem cells from the skin cells of Gaucher patients with and without Parkinson's disease in the lab. She then converted the stem cells into neurons that had features that were identical to those in people with Gaucher disease. Neurons are nerve cells that transmit information via chemical messengers and electrical signals.
The researchers showed that the neurons from Gaucher patients, who also had Parkinson's disease, showed elevated levels of alpha-synuclein. This is the protein that accumulates in the brains of people with Parkinson's disease impacting neurons responsible for controlling movement.
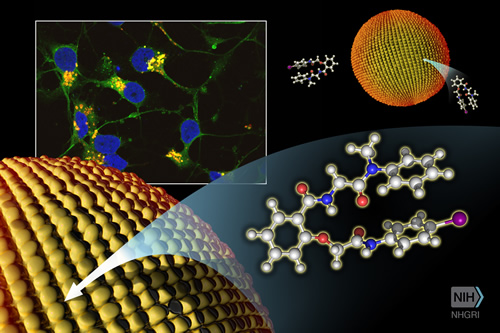
The researchers then looked for a molecule that would help patients with mutant GBA1 break down cellular waste. In a process known as high-throughput drug screening, researchers at NCATS Chemical Genomics Center evaluated hundreds of thousands of different molecules. NCATS researchers Juan Marugan, Ph.D., Samarjit Patnaik, Ph.D., Noel Southall, Ph.D., and Wei Zheng, Ph.D., identified a promising molecule, NCGC607, in conjunction with researchers at the University of Kansas, Lawrence, which helps to "chaperone" the mutated protein so that it can still function. In the patients' stem cell-derived neurons, NCGC607 reversed the lipid accumulation and lowered the amount of alpha-synuclein, suggesting a possible treatment strategy for Parkinson's disease.
"This research constitutes a major advance," said Daniel Kastner, M.D., Ph.D., NHGRI scientific director anddirector of the institute's Division of Intramural Research. "It demonstrates how insights from a rare disorder such as Gaucher disease can have direct relevance to the treatment of common disorders like Parkinson's disease."
Researchers will next test the new molecule to see if it might be developed into an appropriate prototype drug for patients with Gaucher disease and Parkinson's disease.
Gaucher disease affects an estimated 1 in 50,000 to 1 in 100,000 people in the general population. People of Eastern and Central European (Ashkenazi) Jewish heritage are more likely to get Gaucher disease. Parkinson's disease affects 1.5-2 percent of people over age 60, and the incidence increases with age. In the United States, about 60,000 new cases are identified each year. Parkinson's disease affects more than 1 million people in North America and 7-10 million people worldwide.
Read the study
Elma Aflaki, Daniel K. Borger, Nima Moaven, Barbara K. Stubblefield, Steven A. Rogers, Samarjit Patnaik, Frank J. Schoenen, Wendy Westbroek, Wei Zheng, Patricia Sullivan, Hideji Fujiwara, Rohini Sidhu, ZaydMKhaliq, Grisel Lopez, David S. Goldstein, Daniel S. Ory, Juan Marugan, and Ellen Sidransky. A New Glucocerebrosidase Chaperone Reduces α-Synuclein and Glycolipid Levels in iPSC-Derived Dopaminergic Neurons from Patients with Gaucher Disease and Parkinsonism. The Journal of Neuroscience, July 12, 2016
NHGRI is one of the 27 institutes and centers at the NIH, an agency of the Department of Health and Human Services. The NHGRI Division of Intramural Research develops and implements technology to understand, diagnose and treat genomic and genetic diseases. Additional information about NHGRI can be found at: www.genome.gov.
NINDS (http://www.ninds.nih.gov) is the nation's leading funder of research on the brain and nervous system. The mission of NINDS is to seek fundamental knowledge about the brain and nervous system and to use that knowledge to reduce the burden of neurological disease.
About the National Center for Advancing Translational Sciences (NCATS): NCATS is a distinctly different entity in the research ecosystem. Rather than targeting a particular disease or fundamental science, NCATS focuses on what is common across diseases and the translational process. The Center emphasizes innovation and deliverables, relying on the power of data and new technologies to develop, demonstrate and disseminate advances in translational science that bring about tangible improvements in human health. For more information, visit https://ncats.nih.gov.
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.

 ]
]